Anatomic Posterior Cruciate Ligament Reconstruction State of the Art
Review Article
Anatomic anterior cruciate ligament reconstruction for adolescent patients with open up physis
Introduction
In the by, anterior cruciate ligament (ACL) injuries in patients with open physes were mainly managed non-operatively or by suture repair, which also frequently resulted in unsuccessful outcomes (1,2). At that time, the diagnostic possibilities were inferior to electric current standards, and the consequences of pediatric ACL tears and the iatrogenic take chances of pediatric ACL reconstruction had not securely been evaluated yet. Many pediatric ACL injuries were diagnosed late, so that the orthopedic surgeons dealt predominantly with a negative option of ACL-injured children, who presented with secondary meniscal tears and cartilage lesions. Today, pediatric ACL reconstruction (ACLR) is considered a prophylactic procedure with low complication rates, provided that surgery is performed correctly (3,iv). However, the issue after ACLR in children and adolescents is poorer in comparison to adults, which suggests to carefully evaluate each patient before confirming the indication for surgery and to avert treating all pediatric ACL injuries surgically on a systematic footing (3). Indication for surgery needs to be tailored to each patient, and should be based on clinical factors similar functional instability, associated injuries, remaining knee growth and patient expectations.
Recently, international guidelines on the direction of pediatric ACL injuries accept been published by the International Olympic Commission (IOC), in partnership with international scientific organizations similar ESSKA, AOSSM, SLARD, APKASS and ISAKOS (5,6). Non-operative treatment with a structured rehabilitation program has shown to be successful in some patients (7). Still, a strong association between the filibuster of surgery and the occurrence of meniscus and cartilage lesions has been reported, suggesting that an uncontrolled non-operative treatment may be detrimental to the intra-articular soft tissue structures (one,ii,8-ten). Therefore, since the immature ACL-deficient knee can evolve with patient's growth, regular follow-up visits with clinical investigation, magnetic resonance imaging (MRI) and laxity testing are indicated (eleven). Pediatric ACL surgery is highly specialized, due to the specific beefcake of children'southward knees and its serious complication potential (12-17). Surgical results are expert, but seem to exist less predictable than in adults (18-22). Furthermore, in that location are not enough high-quality result studies later surgical treatment (three). The goal of this article is to provide a concise overview on the state of the fine art of pediatric ACL injuries.
Epidemiology
ACL tears in children and adolescents with open growth plates (Figure 1) account for less than 5% of all ACL injuries (24-26). They exercise rarely occur before the age of nine and three out of four are sports injuries (20). The number of pediatric ACL tears seems to be rising over the years. Between 1994 and 2013 a hateful annual increase of pediatric ACL tears of 2.3% was reported in the USA (27), whereas in Victoria, Australia, the overall annual rate of hospital-treated ACL injuries increased past 147.eight% between 2005 and 2022 (28). This dramatic increase is caused by the physicians' improved clinical and diagnostic skills (27-29), the growing popularity of high-risk sports in children and adolescents (five,28,thirty,31), and potentially also the decreasing motor skills in this young population (32). In a non-able-bodied adult population, the incidence of ACL injuries is budgeted the 0.ane% rate (33-35). Information from populations of young athletes are rare. In a sports school including young athletes from various sports disciplines, we identified an incidence approaching the i% rate (non-published information).
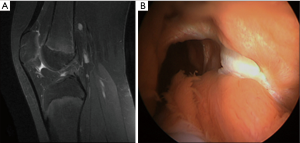
Figure 1 ACL tear in the right knee of an 11-yr-old male child. Sagittal view on MRI (A), arthroscopic view with empty lateral wall (B). Reprinted by permission from (23). ACL, inductive cruciate ligament.
Clinical presentation
Usually, the ACL tear it is a issue of a noncontact injury involving cutting, pivoting or rapid deceleration. Valgus twisting is the almost common injury mechanism, but pure internal rotation of the tibia on the femur and hyperextension of the knee can also be involved.
In an astute setting, ACL injuries are often associated with intense pain and haemarthrosis, which tin impede a precise test. The non-injured knee should always be tested in guild to appraise physiologic laxity, frequently more of import in skeletally young patients than in adults. The assessment of the range of motion can testify loss of extension in case of displaced bucket-handle meniscal tears, chondral or osteochondral fragments or arthrofibrosis. The loss of flexion can be caused past the haemarthrosis. Joint line tenderness and positive McMurray, Apley or Childress tests can suggest a meniscal tear. Localized pain on the tibial or femoral collateral ligaments attachment sites, associated with positive varus or valgus stress tests can be signs of associated ligamentous injuries. The clinical examination should also include the evaluation of the extensor mechanism, patellar tracking and stability, the posterior cruciate ligament (PCL) and the collateral ligaments. The ACL is evaluated with the Lachman test, the anterior drawer and the pivot shift test, which is not always easy to assess in pediatric patients. Since clinical symptoms and presentations may vary at dissimilar fourth dimension point after injury, tests should be repeated at every follow-up visit. To confirm and document the diagnosis, the pivot shift test should exist done systematically also in the operating room under full general anesthesia in case of surgery. Lower extremity alignment and limb length should also exist documented. In the absence of fractures, patellar dislocations and built meniscus lesions need to be ruled out as main differential diagnosis.
Imaging
Standard radiographs including anteropostetior (AP), strict lateral and skyline views are the showtime diagnostic workup in severe knee injuries in children. MRI is mandatory in case of suspected ACL tear; however, identification of this injury is more difficult in children as compared to adults, with a sensitivity of 62% and a specificity of xc% in children nether the age of 12 (36,37). From 12 to 16 years, sensitivity and specificity increment to 78% respectively 96% (38). Secondary MRI features like subchondral bone bruise are less frequently identified in children, owing to the inherent increased laxity of pediatric knees.
General therapeutic considerations (strategy)
Goals of pediatric ACL tears treatment are to restore a stable, well-functioning knee, enabling an active lifestyle, to reduce the affect of existing meniscal or chondral pathology, the run a risk of further degenerative joint changes and the need for hereafter surgery and minimize the risk of growth disturbances and deformity. Surgery for pediatric ACL tears is indicated in instance of associated meniscus or cartilage lesions, recurrent, symptomatic giving fashion and unacceptable restriction in participation to sports or recreational activities.
Acute ACL surgery is rarely indicated. Associated meniscus lesions or cartilage injuries may support the need of an acute ACL reconstruction, especially in case of a confused bucket-handle meniscus tear or a large osteochondral fleck fracture. Physicians should acquit in mind that a patient referred for a confused meniscus saucepan handle tear may have an underlying, previously undiagnosed ACL injury. ACL reconstruction may be considered in the presence of no or just minor swelling and synovitis; of capital importance are, an experienced surgical surround and fully informed young patients and parents. They demand to exist aware of the complication potential and the need for a close clinical follow-up until the end of the growth period. Because of their unfavorable results with respect to recurrent injuries, isolated meniscus repair without associated or subsequent ACL reconstruction cannot be recommended.
In all other cases, bracing and a home-based rehabilitation program are encouraged. This tin can be a short-term selection to delay surgery until skeletal maturity is reached or a permanent treatment if no further disease progression is observed. For isolated ACL injuries, a structured rehabilitation programme should be applied and priority should exist given to regain complimentary range of motion and a pain free, not-swollen knee. In non-operated knees, physical activity tin be regained progressively over a iii to 6 months' menstruation (five). Return to level 1 sports (sports with frequent pivoting and contact, e.yard., soccer, handball, basketball) (39) should be considered with circumspection. In children with lower ambitions, changing physical activity to level 2 sports (mostly individual sports with less frequent pivoting than level I sports, due east.chiliad., dissonance sports, alpine skiing, snowboarding, gymnastics and aerobics) (39) is considered a safer selection.
If a decision for a longer-term nonoperative handling is called, we perform a systematic follow up with almanac MRI's to evaluate the meniscal status also as the development of the PCL angle. The PCL angle is determined as the angle between the lines drawn through the central portion of the tibial and femoral insertions of the PCL. A PCL angle of <105° is considered suggestive of an ACL injury due to a chronic anterior drawer of the tibia in relation to the femur (11,36). Progression of meniscal lesions and PCL bending on MRI signal the decompensation of an ACL-deficient human knee with a chronic anterior drawer (Figures ii,3), which warrants surgical treatment. Also, lateral monopodial stance radiographs at xv° of flexion of the injured and contralateral knee joint may exist used to evaluate side-to-side differences in spontaneous anterior drawer (xl).

Figure 2 Progression of a complex meniscal lesion, with associated formation of a meniscal cyst and posterior subluxation of the lateral meniscus, afterward pediatric ACL tear (nine years old boy) treated conservatively. (A) Iii years after ACL tear; (B) iv years later ACL tear; (C) 4 years and 6 months after ACL tear. The posterior horn of the lateral meniscus is indicated with an arrowhead. Technique: sagittal reconstructions in proton-density fatty-saturation sequences of the right knee joint, centred on the posterior horn of the lateral meniscus. ACL, inductive cruciate ligament.

Figure three Progressive reduction of the PCL bending afterwards pediatric ACL tear (9 years erstwhile boy) treated conservatively. (A) 3 years after ACL tear; (B) 4 years after ACL tear; (C) four years and 6 months after ACL tear. A PCL bending of <105° is considered suggestive of an ACL injury. Technique: sagittal reconstructions in proton-density fat-saturation sequences of the correct human knee, centred on the PCL. PCL, posterior cruciate ligament; ACL, anterior cruciate ligament.
Remaining functional instability with recurrent giving way episodes despite the structured rehabilitation plan is another indication for surgery. Surgeons must be aware that younger children may not recognize or describe them every bit such and specific questioning may therefore be required. In the surgical decision-making process, the child'due south private needs and maturation process, including remaining growth based on skeletal historic period determination must be considered. As well, ethical standards to guide shared decision making must exist taken into consideration in ambitious young athletes (41).
Knee growth, maturation and preoperative planning
Systematic preoperative planning is mandatory in young individuals. Standard radiographs should include AP, lateral and patellofemoral views, also as an AP view in 45° of knee flexion (Figure 4). Determination of the skeletal historic period and the remaining growth potential past using Ten-rays of the left hand and wrist and the Greulich and Pyle tables is recommended. Boosted methods such as pelvic or elbow X-rays tin complement the Greulich and Pyle method and can be more accurate in certain patients during puberty (42,43). Newer MRI based methods of bone age assessment will need farther validation (44).
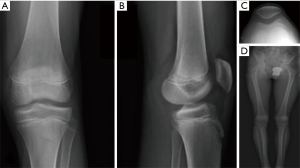
Figure 4 A standardized series of radiographs is required for the preoperative planning of an ACL reconstruction in children, which includes: AP (A) and lateral (B) views, patellofemoral view (C), full leg view (D). Reprinted by permission from (23). ACL, anterior cruciate ligament; AP, anteroposterior.
Lower limb continuing radiographs should be obtained for documentation of alignment as well as to rule out preoperatively existing limb length discrepancies. If bachelor, depression-dose irradiation long leg standing radiographs (e.g., with the EOS arrangement) should be preferred to standard techniques (45).
Knowledge of the remaining human knee growth is of utmost importance. In this respect, the knee growth and maturation chart (Figure 5), can be a useful tool (47). It is based on the growth speed of the physeal plates at the knee and the skeletal age and allows differentiating betwixt 3 unlike periods: (I) a first, prepubertal phase, in which the growth potential of the distal femoral and the proximal tibial physis are nevertheless high. The end of this phase occurs approximately at the age of 13 in girls and 15 in boys. At this stage, pediatric surgical techniques should exist considered; (Two) a second, pubertal phase, with a decreasing physeal growth potential, the duration of which approximates ane yr (thirteen–14 years old in girls and xv–16 years former in boys). Pediatric surgical techniques are also recommended at this stage, because growth plate injuries notwithstanding can crusade significant growth abnormalities; (Iii) the final developed phase starts at 14 years old in girls and 16 years old in boys. At this moment, growth plate closure has occurred at the distal femur and the proximal tibia and adult procedures tin can be used.
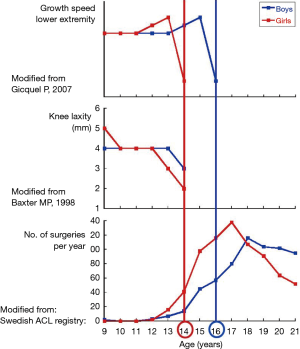
Figure five The superposition of three tables shows the growth velocity of the knee physes in relation to the skeletal age. This diagram allows a quick categorization of patients before surgery. The pinnacle graph depicts lower limb growth velocity with respect to the patients' age (46). During growth (rapid acceleration stage), the growth plates around the knee accept a high growth velocity of about 2 cm/twelvemonth. The use of pediatric ACL reconstruction techniques is mandatory in this stage. From the historic period of xiii in girls and 15 in boys, the growth velocity decreases chop-chop (gradual deceleration phase) until the growth of the lower limb stops: this occurs at the age of 14 in girls and 16 in boys. From this time indicate on, developed ACL-reconstruction techniques can be used. The middle graph shows the subtract of physiologic knee laxity every bit reported past Baxter (47). A decrease in laxity corresponds to the concluding phase of human knee growth. The lower graph represents the numbers of ACL surgeries performed in Sweden in 2010. It confirms the clinical experience that the frequency of ACL injuries increases afterward the stop of genu growth, one time the knees have stiffened. Reprinted past permission from (23). ACL, anterior cruciate ligament.
Surgical techniques
Many ACL reconstruction techniques have been described in children and adolescents. Their goal is to reproduce ACL anatomy the all-time possible and to reduce iatrogenic complications to a minimum. Due to the presence of the distal femoral and proximal tibial growth plates, anatomic graft placement is difficult to obtain in children with the currently available techniques (48). With respect to tibial and femoral tunnel placement, surgical techniques tin be divided into three categories (Figure 6): (I) transphyseal procedures, in which the tunnels are drilled through the growth plates—this is the author's preferred technique, even in prepubertal and pubertal patients—(II) epiphyseal techniques, in the growth plate is not injured, since the tunnels are located in the tibial and femoral epiphysis, and (III) extraepiphyseal techniques, in which the graft is placed around the growth plate. The graft can be placed in different techniques both on the tibial and the femoral side. Every surgical strategy bear potential for specific complications. To increase the condom and reproducibility of the surgical procedures and minimize the hazard of affecting future normal growth, general surgical guidelines have been established (49) (Table i).
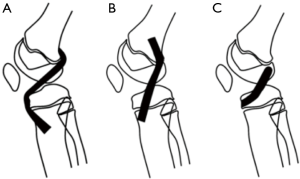
Figure vi Schematic representation of unlike techniques for ACL reconstruction in pediatric patients. (A) Growth plate preserving technique (extraepiphyseal). The graft is passed around the tibial and the femoral physis; (B) transphyseal technique. The graft is passed through the tibial and femoral physis; (C) growth plate preserving technique with epiphyseal tunnels. A large number of variations to these techniques have been described. Adapted by permission from (23). ACL, anterior cruciate ligament.

Tabular array 1 Fourteen recommendations for preoperative planning and surgery for pediatric ACL reconstructions [adapted from (49)]
Full tabular arrayThe different graft types which are used in adults may besides exist used with some modifications in children. Hamstring grafts are the most popular (49,50). In some cases, their diameter can be besides minor to reproduce a graft bore of 6–viii mm (51). Unfortunately, preoperative conclusion of the graft bore is unreliable and therefore they may be reinforced with other tendon textile (e.g., by a quadriceps strip) if this situation would occur unexpectedly during surgery (51,52). In order to prevent injuring the growth plate of the tibial tuberosity which can be the cause of a recurvatum knee joint in case of growth abort, it is important not to impairment the tibial periosteal zipper of the hamstrings. Unlike the adult harvesting technique, information technology is recommended to detach the hamstrings tendons proximal to their bony insertion site, leaving the tibial zipper site intact. Quadriceps and patellar tendon grafts remain a valid option likewise in pediatric ACL reconstruction: in this case, it is recommended to harvest them without a os cake. If a bone block is role of the technique (eastward.g., in an epiphyseal process), the placement of the cake through the growth plate must be absolutely avoided, since it can cause early growth plate fusion. The iliotibial band is a further option as a graft material, especially if an extraepiphyseal, extraarticular technique is performed (53). Care should be taken to inform the patient on potential cosmetic (big incision) and harvesting site problems (pain). A general consensus in the IOC recommendations has been expressed against the use of cadaver allografts in young children, which should be avoided due to poor clinical outcomes (5). Living-donor hamstring tendon allografts may accept certain advantages over the cadaver allografts only they enhance ethical questions and long-term outcomes still need to be assessed (54,55). The use of synthetic graft material is prohibited in pediatric ACL reconstruction, since it may cause significant growth abort.
Some authors differentiate their specific pediatric ACL reconstruction technique co-ordinate to the amount of human knee growth remaining. They recommended extraphyseal reconstruction techniques for very young patients, transphyseal reconstruction for older patients, and partial transphyseal procedures in between (51,56,57). The background for this strategy is based on the theoretical age-related risk of growth abort represented by the principle that the extent of a possible deformity is inversely proportional to the patient's historic period. However, information technology was noticed that the probability for growth abnormalities to occur existed mainly in adolescents during the concluding yr before knee physeal closure (20). This may be related to the high capacity of the growth plate to break small-scale epiphyso-metaphyseal os bridges spontaneously in young children, a capacity which is slowing downwards with the maturation process (58). In others words, the amount of potential growth deformity is modest in older children, merely the risk for a growth arrest to occur may be much college. For this reason, we believe that when a patient'southward knee is close to skeletal maturity, delayed reconstruction may exist considered (59). At the other finish of the spectrum, in the prepubertal stage, there is sufficient testify that transphyseal techniques are condom (sixty), provided that the technical recommendations for these procedures are respected (49).
In guild to minimize the risk of growth disturbance, Kocher advocated a physeal-sparing combined intra-articular and actress-articular reconstruction with an autologous iliotibial band in prepubescent (Tanner stage 1 or 2) children with a large amount of growth remaining (21,22). In pubescent adolescents with growth remaining (Tanner stage 3), they recommended a transphyseal hamstring graft technique with extracortical fixation (22). A similar technique is used by the authors on a routine basis even in prepubescent children (Figure 7) (61). It does not differ drastically from ACL reconstructions in the developed patient. The diameter of the graft usually varies between half dozen and 8 mm. To minimize the drill injury in prepubescent children under the historic period of 10, a transtibial technique is preferred for the femoral tunnel. It allows creating a more perpendicular femoral tunnel in relation to the distal femoral physis. In children older than 10, with still significant knee growth remaining, the femoral tunnel is drilled through the anteromedial portal after having placed the human knee in maximal flexion. While this induces a greater drill injury, it allows obtaining a more anatomic placement of the femoral graft. The use of a femoral drill guide with a 5-mm or even a vii-mm starting time tin be considered to prevent a blowout of the posterior cortex of the femur and to avert injury of the perichondral structures (Figures 8,9). On the tibial side, care must be taken to position the tunnel entrance more than medially as it is done in adults. It helps to protect the apophysis of the tibial tuberosity (located laterally to the tunnel entry point) likewise as to avert subsequent development of a growth arrest with a secondary recurvatum deformity (62). An arthroscopically assisted technique which combines a transphyseal drilling on the tibial side and an intraepiphyseal drilling on the femoral side has been proposed past Henry et al. (nine). In this technique, a quadriceps tendon graft with a trapezoidal bone block is used. A pin is inserted under fluoroscopic guidance to ensure that the femoral tunnel is drilled parallel and at a prophylactic altitude from the physis. An exterior-in technique is so used and the graft is introduced. The bone block is impacted press-fit in the femoral tunnel. Double tibial fixation is obtained by combining by an extracortical staple and a biodegradable screw in the tunnel which is placed distal to the tibial physis. The so-called Clocheville technique is an example of a nonanatomic, extraphyseal technique, in which the mid-third of the patellar tendon is used, without os blocks (eighteen,24,63). Instead of these, a periosteal flap is harvested at both the tibial and the patellar insertion sites. The femoral tunnel is positioned proximally to the growth plate, whereas on the tibial side, the graft is fixed at the epiphysis in a os trough, which has a depth of 1 cm. This procedure has been used for many years, peculiarly in very young, prepubertal children, although it is technically more demanding than the arthroscopic single tunnel technique.
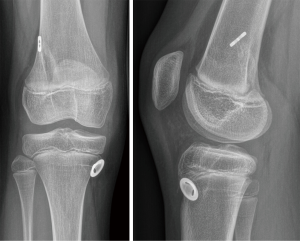
Figure seven Postoperative AP and lateral views of a 9-yr-old girl who tore her ACL during alpine skiing. Afterwards nonoperative treatment was considered, she adult recurrent giving way, so that surgery become necessary. A 4-fold transphyseal semitendinosus-gracilis reconstruction with extracortical fixation was performed. Reprinted by permission from (23). ACL, inductive cruciate ligament; AP, anteroposterior.
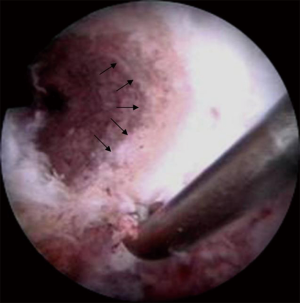
Effigy 8 Arthroscopic view of the right knee of a 12-year-former boy: the femoral tunnel is showed subsequently drilling to perform an ACL reconstruction, with the probe placed at the over-the-elevation position. The distal femoral physis is visible (arrows). The picture demonstrates the shut proximity of the dorsal femoral tunnel to the periphery of the growth plate. Reprinted by permission from (23). ACL, inductive cruciate ligament.

Figure ix Schematic representation of the tibial and femoral tunnels after a transphyseal ACL reconstruction in a 10-year-erstwhile girl. On the tibial side, a stronger verticalization of the tunnel could reduce the surface area of injury to the growth plate. On the femoral side, the crimson betoken marks the femoral insertion of the ACL. It is merely 3 mm abroad from the ossification groove of Ranvier. In gild to protect this structure, a drilling guide with a 5-mm start was chosen. With a tunnel diameter of 6 mm, there is at to the lowest degree a 2 mm safety margin between the posterior wall of the tunnel and the groove. Reprinted by permission from (23). ACL, anterior cruciate ligament.
Recent anatomical studies suggested a part of the anterolateral ligament of the knee in common knee instability patterns (64). Sure authors propose therefore lateral extra-articular tenodesis equally a method of ACL graft protection and knee stabilization for adult patients with high-grade pivot shift examination, in chronic ACL rupture, young patients, pivoting activities, and patients undergoing medial meniscus repair (65). There is currently no consensus regarding the use of this technique in skeletally immature patients.
Growth plate injury and potential complications
Growth disturbances later ACL reconstruction are underreported (50). They evolve throughout the entire procedure of remaining growth. The type and corporeality of the deformity are proportional to the localization and the size of the initial growth plate injury as well as the patient's remaining growth potential.
Growth disturbances after ACL reconstruction can exist categorized into 3 groups (66). Growth abort (A) is caused by a localized injury of the growth plate, which activates the formation of a transphyseal os bridge. If this growth arrest is located at the periphery of the physis, it may lead to axial deformities. If information technology is located in the center of the growth plate, information technology can lead to symmetrical leg length discrepancies. In very immature children the growth plate tin create distraction forces fifty-fifty later on the creation of a transphyseal bone bridge, so that a spontaneous breakage of the span may occur. Bone bridge germination can be prevented if a soft tissue graft crosses the growth plate injury. Transphyseal placement of a os cake, hardware or synthetic graft placement should be avoided to avoid sudden growth arrest. Peripheral growth plate injuries to the distal femoral plate can also exist provoked using a transphyseal technique if the tunnel is as well big or if there is a posterior accident-out with subsequent injury of the perichondral structures of the growth plate (Ranvier zone and perichondral ring of Lacroix). Growth plate injuries cannot be avoided using epiphyseal technique. The former volition exist much larger as compared to those possible with a transphyseal technique: asymmetric growth in these cases can exist much more than astringent in comparison to an arrest caused by transphyseal drilling; for this reason, tunnel drilling should always be performed under fluoroscopy to ensure that the femoral tunnel is located distally to the growth plate. When considering extraphyseal (over the top) techniques, extreme care is necessary to avert an excessive rasping of the over the top position. This surgical maneuver is used to obtain a better graft adhesion, but may crusade injuries to the perichondral structures and lead to centric malalignment. Since injuries using this technique occur in a posterolateral position, a growth arrest at the femoral tunnel site volition atomic number 82 to a deformity in valgus and flexion. In these cases, the amount of deformity tin can be predicted anticipating the remaining growth allows. On the tibial side, peripheral injuries may be acquired if the tibial tuberosity apophysis is damaged, either during harvesting of the hamstring tendons or if the tibial tunnel archway is created in a too inductive position: a recurvatum of the proximal tibia will result from a growth arrest in this region.
Focal physeal disruptions after transphyseal ACL reconstruction in adolescents with open physis were evaluated past Yoo et al. In 5 of 43 adolescent patients' disruption was observed in MRI, although without any clinical consequences, so that the authors ended that transphyseal techniques are not harmless and should not be used in immature children (58). In contrast to this decision, nosotros believe that in younger children those focal os bridges volition break easily, so that these patients will bear a lower adventure of epiphysiodesis every bit compared to adolescents (59). In whatever case, the risks of a procedure and its consequences are concepts which cannot be assimilated: in fact, adolescents are at a higher risk of epiphysiodesis, merely this has, in their age, limited clinical consequences in terms of a disturbance in hereafter limb growth. On the other paw, the chance of epiphysiodesis in young children is low, but this even has sometimes dramatic clinical consequences if a physeal bridge persists and continues to develop until the end of growth.
The second type of growth abnormality is an overgrowth process (type B: heave). Boosts occur mainly in very young children and are likely to be caused past a local hypervascularization, which stimulates the physeal growth process. The growth disturbance volition become apparent inside a limited period of 2 years following surgery. It normally has a symmetric form and may lead to a moderate leg length discrepancy. McIntosh et al. reported a leg length discrepancy of less than ten mm in fifteen out of 16 patients. Only 1 patient had the operated limb 15 mm longer than the good for you limb (67). As compared to a full growth abort, the clinical impact of overgrowth is unremarkably low. Notwithstanding, the demand of a percutaneous epiphysiodesis has been reported considering of a provisional leg discrepancy effectually two centimeters in an viii-year-onetime kid at the time of ACL reconstruction (66). A tibial valgus deformity can sometimes besides occur, due to asymmetrical overgrowth. This is similar to a posttraumatic genu valgum, the deformity observed after metaphyseal pediatric proximal tibial fractures. After an initial progressive increment of the deformity, a spontaneous correction tin all the same occur, a shut follow-upwards with nonoperative handling of the deformity is therefore recommended (66).
The third blazon of growth disturbance is a deceleration of the remaining growth (type C: decelerate), which may be acquired by a so-called "tenoepiphysiodesis" result due to an excessive graft tension across the physis (xiii). Up to engagement, it is not nonetheless articulate which is the exact amount of graft tension necessary to cause such an abnormality in humans. Animate being studies have demonstrated that it should not exceed 80 N. The use of a non-biological, synthetic graft is expected to produce the same effect. The mechanism underlying this growth aberration is chosen Hueter-Volkmann principle, which affirms that an excessive pressure directed on the growth plate reduces the longitudinal growth, and vice versa.
To detect in a timely fashion whatever possible growth abnormality, a much stricter post-operative follows upward is recommended for children, as compared to adults: clinical and radiological controls are mandatory until the end of the growth. If a permanent growth abnormality is discovered, the cause of which is clearly identified (i.e., transphyseal hardware or bone block placement), immediate surgical revision is recommended. A Langenskiöld procedure (soft-tissue interposition) or an boosted epiphysiodesis may be considered. On the other hand, if operative revision is not considered immediately, a correction osteotomy using specific plates or Ilizarov fixators can be necessary at the finish of the growth period. Fortunately, the incidence of these complications is extremely depression, especially if surgery was properly performed. Nevertheless, before surgery the children and their parents must exist informed on their possible occurrence, even in experienced easily.
Rehabilitation and render to sports
Rehabilitation guidelines differ for prepubescent children and adolescents who are close to skeletal maturity. Whereas adolescents may follow rehabilitation and return-to-sports-principles and guidelines which are intended for adults, specific considerations accept been recommended in the IOC consensus for children. In general terms, rehabilitation is similar irrespective of the surgical technique, although more carefully handled than in adults. Weight bearing is immune from the first, with an exception for associated cartilage repair procedures or some types of meniscal repair (e.g., radial tear or meniscus root repair). In instance of an associated meniscus repair, an extension caryatid is commonly recommended over a period of 6 weeks. Motion must be started early to avoid arthrofibrosis (68).
Functional tests, criteria to evaluate movement quality and return to sports criteria have not been validated in children then far. A recent multicenter investigation from the French Arthroscopy Society analyzing graft indicate intensity after pediatric ACLR in 126 prepubescent children (skeletal age <13.v years in girls and <15.5 years in boys) revealed that return to sports should exist more than conservative in children in comparison to adults. Investigators looked at graft changes on MRI upwards to 2 years' post-surgery (69). They found an absence of bespeak normalization of the ACL graft with inhomogeneous indicate-to-noise quotient and lower Howell grades than those which tin be found in adults.
Results, clinical outcomes and first registries
Providing a complete overview of clinical results after pediatric ACL surgery would be beyond the scope of this article. Therefore, this chapter was restricted to two major reviews. The starting time analyzed the quality of published studies and the second analyzes the clinical results and complications.
Due to widespread methodological deficiencies of many of the studies on the treatment of pediatric ACL injuries, Moksnes et al. advised caution when interpreting results (3). No randomized controlled trials and just few prospective cohort studies are currently bachelor in the literature (7,seventy). Operated patients considered in these studies could represent a negative selection of all ACL injured skeletally young patients inducing a potential bias. The methodological quality of 31 studies investigating the event of the treatment of ACL injuries in skeletally immature individuals was recently evaluated past the Coleman Methodology Score, which tin range from 0 to 100 (maximum) (71). The authors identified only four studies with a score of 60 or more (maximum 64), so that they concluded defining equally low current treatment prove of ACL injuries in children.
L-5 manufactures with 935 patients (median age 13 years) were included in a meta-analysis of case series (level of evidence Iv) of pediatric patients undergoing ACL reconstruction by Frosch et al. The median follow-up of 40 months (range 14 to 89 months), after which leg-length discrepancies or axial malalignments were documented in 1.8% of the cases (threescore). Excellent or good role, indicated by an International Articulatio genus Documentation Committee grade A or B, was obtained in 84.two% of all knees, and the average Lysholm scores was 96.3. Approximately five% of re-ruptures occurred. The gamble of leg-length differences or centric malalignment was significantly lower in transphyseal reconstructions when compared with physeal-sparing techniques. However, the hazard of recurrent tears was higher for the transphyseal reconstructions (four.two% vs. i.four%). The authors concluded suggesting the need of randomized controlled trials to analyze these issues in the management of ACL injuries in children and adolescents.
In society to overcome the intrinsic limits of regional example studies and to provide a stronger footing to scientific cognition, two registries take been developed, which monitor the outcomes of pediatric ACL treatment. The PLUTO (Pediatric ACL: Understanding Treatment Outcomes) is a multi-eye, prospective cohort study started in 2022 nether the lead of the Boston Children's Infirmary, which aim is to evaluate the safe and effectiveness of non-operative treatment, as well equally four operative treatments including transphyseal, fractional transphyseal, and physeal-sparing techniques (72). The PAMI (Paediatric Anterior Cruciate Ligament Monitoring Initiative) is a recently started pan-European system for the collection and assay of data from orthopaedic surgeons who are treating children and adolescents with ACL injuries, aimed at collecting short-, medium- and long-term clinical outcome of bourgeois and surgical handling and at proposing internationally accepted treatment guidelines (50).
Conclusions
The knowledge of pediatric ACL injuries and their treatment has fabricated significant progress over the terminal iii decades. Over the years, specific pediatric surgical techniques were developed and optimized. They proved to exist successful and safety if used in a technically correct fashion. Nowadays, although pediatric techniques are used on a larger scale, surgery notwithstanding maintains challenging aspects, particularly due to the specific characteristics of the pediatric patient. Surgery-related complications occur, but their frequency has dropped to an acceptably low level (<2%). In the last decade, attention to nonoperative handling likewise increased, which helped refining the indications for conservative handling. Information technology is estimated that 30–l% of patients could benefit from nonoperative treatment, whereas others may develop rapidly secondary soft-tissue injuries requiring surgery. A close follow upwards of pediatric patients is therefore recommended. Equally pediatric ACL injuries are increasingly recognized and as physicians are confronted with many unlike situations at different evolutionary stages, continuous progress is now required to select the correct treatment at the right moment for the appropriate patient.
Acknowledgments
Funding: None.
Provenance and Peer Review: This article was commissioned by the Guest Editor (Takeshi Muneta) for the serial "Anatomic Reconstruction of Inductive Cruciate Ligament - Concept, Indication, and Its Efficacy" published in Register of Joint. The commodity has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (bachelor at http://dx.doi.org/10.21037/aoj.2019.06.02). The series "Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy" was commissioned by the editorial office without whatever funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are answerable for all aspects of the work in ensuring that questions related to the accurateness or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open up Access commodity distributed in accordance with the Artistic Commons Attribution-NonCommercial-NoDerivs iv.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/past-nc-nd/4.0/.
References
- Mizuta H, Kubota Thou, Shiraishi M, et al. The bourgeois treatment of complete tears of the anterior cruciate ligament in skeletally young patients. J Bone Articulation Surg Br 1995;77:890-4. [Crossref] [PubMed]
- Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: Does a filibuster in treatment increase the risk of meniscal tear? Arthroscopy 2002;18:955-9. [Crossref] [PubMed]
- Moksnes H, Engebretsen 50, Risberg MA. The current evidence for treatment of ACL injuries in children is depression: a systematic review. J Os Joint Surg Am 2012;94:1112-9. [Crossref] [PubMed]
- Peterson DC, Ayeni OM. Pediatric anterior cruciate ligament reconstruction outcomes. Curr Rev Musculoskelet Med 2016;9:339-47. [Crossref] [PubMed]
- International Olympic Commission Pediatric ACL Injury Consensus Grouping. 2022 International Olympic Commission Consensus Statement on Prevention, Diagnosis, and Management of Pediatric Anterior Cruciate Ligament Injuries. Orthop J Sports Med 2018;6:2325967118759953 [PubMed]
- Seil R, Theisen D, Moksnes H, et al. ESSKA partners and the IOC join forces to amend children ACL handling. Knee Surg Sports Traumatol Arthrosc 2018;26:983-4. [Crossref] [PubMed]
- Moksnes H, Engebretsen Fifty, Eitzen I, et al. Functional outcomes following a not-operative treatment algorithm for inductive cruciate ligament injuries in skeletally young children 12 years and younger. A prospective cohort with 2 years follow-up. Br J Sports Med 2013;47:488-94. [Crossref] [PubMed]
- Dumont GD, Hogue GD, Padalecki JR, et al. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: human relationship of treatment time and patient-specific factors. Am J Sports Med 2012;40:2128-33. [Crossref] [PubMed]
- Henry J, Chotel F, Chouteau J, et al. Rupture of the inductive cruciate ligament in children: early reconstruction with open physes or delayed reconstruction to skeletal maturity? Knee Surg Sports Traumatol Arthrosc 2009;17:748-55. [Crossref] [PubMed]
- Lawrence JTR, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an inductive cruciate ligament tear: is there harm in delay of handling? Am J Sports Med 2011;39:2582-seven. [Crossref] [PubMed]
- Cucchi D, Mouton C, Dor, et al. Paediatric ACL tear. In: Tapasvi S, Shekhar Due south. Knee Arthroscopy: A Example Repository. New Delhi, Bharat: Jaypee Brothers Medical Publishers (P) Ltd., 2019.
- Anderson AF. Transepiphyseal replacement of the inductive cruciate ligament in skeletally immature patients. A preliminary report. J Bone Joint Surg Am 2003;85:1255-63. [Crossref] [PubMed]
- Edwards TB, Greene CC, Baratta RV, et al. The effect of placing a tensioned graft across open growth plates. A gross and histologic assay. J Bone Joint Surg Am 2001;83:725-34. [Crossref] [PubMed]
- Hudgens JL, Dahm DL. Handling of anterior cruciate ligament injury in skeletally young patients. Int J Pediatr 2012;2012:932702 [Crossref] [PubMed]
- Kocher MS, Saxon HS, Hovis West, et al. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Order and The ACL Written report Group. J Pediatr Orthop 2002;22:452-7. [Crossref] [PubMed]
- Seil R, Pape D, Kohn D. The chance of growth changes during transphyseal drilling in sheep with open physes. Arthroscopy 2008;24:824-33. [Crossref] [PubMed]
- Stadelmaier DM, Arnoczky SP, Dodds J, et al. The effect of drilling and soft tissue grafting across open growth plates. A histologic study. Am J Sports Med 1995;23:431-five. [Crossref] [PubMed]
- Bonnard C, Fournier J, Babusiaux D, et al. Physeal-sparing reconstruction of inductive cruciate ligament tears in children: results of 57 cases using patellar tendon. J Bone Joint Surg Br 2011;93:542-7. [Crossref] [PubMed]
- Cassard X, Cavaignac Due east, Maubisson Fifty, et al. Anterior cruciate ligament reconstruction in children with a quadrupled semitendinosus graft: preliminary results with minimum two years of follow-up. J Pediatr Orthop 2014;34:lxx-seven. [Crossref] [PubMed]
- Chotel F, Bonnard C, Accadbled F, et al. Résultats et facteurs pronostiques de la reconstruction du LCA sur genou en croissance. À propos d'une série multicentrique de 102 cas. Rev Chir Orthop 2007;93:131-8. [Crossref]
- Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally young prepubescent children and adolescents. J Bone Articulation Surg Am 2005;87:2371-nine. [PubMed]
- Kocher MS, Smith JT, Zoric BJ, et al. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am 2007;89:2632-9. [Crossref] [PubMed]
- Seil R, Chotel F. ACL Injuries in Children. In: Doral Yard, Karlsson J. Sports Injuries. Copenhagen, Denmark: Springer 2014:1-17.
- Parkkari J, Pasanen 1000, Mattila VM, et al. The risk for a cruciate ligament injury of the genu in adolescents and young adults: a population-based cohort study of 46 500 people with a 9-year follow-up. Br J Sports Med 2008;42:422-6. [Crossref] [PubMed]
- Shea KG, Grimm NL, Ewing CK, et al. Youth sports anterior cruciate ligament and knee injury epidemiology: who is getting injured? In what sports? When? Clin Sports Med 2011;thirty:691-706. [Crossref] [PubMed]
- Seil R, Kohn D. Les ruptures du ligament croisé antérieur chez l'enfant. Balderdash Soc Sci Med Grand Duche Luxemb 2000;1:39-53. [PubMed]
- Beck NA, Lawrence JTR, Nordin JD, et al. ACL Tears in School-Aged Children and Adolescents Over 20 Years. Pediatrics 2017;139:e20161877 [Crossref] [PubMed]
- Shaw L, Finch CF. Trends in Pediatric and Boyish Anterior Cruciate Ligament Injuries in Victoria, Commonwealth of australia 2005-2015. Int J Environ Res Public Health 2017;fourteen:e599 [Crossref] [PubMed]
- Dodwell ER, Lamont LE, Dark-green DW, et al. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med 2014;42:675-80. [Crossref] [PubMed]
- Astur DC, Cachoeira CM, da Silva Vieira T, et al. Increased incidence of inductive cruciate ligament revision surgery in paediatric verses adult population. Knee Surg Sports Traumatol Arthrosc 2018;26:1362-vi. [Crossref] [PubMed]
- Werner BC, Yang Due south, Looney AM, et al. Trends in Pediatric and Adolescent Inductive Cruciate Ligament Injury and Reconstruction. J Pediatr Orthop 2016;36:447-52. [Crossref] [PubMed]
- Myer GD, Faigenbaum AD, Ford KR, et al. When to initiate integrative neuromuscular training to reduce sports-related injuries and enhance health in youth? Curr Sports Med Rep 2011;10:155-66. [Crossref] [PubMed]
- Renström PA. Eight clinical conundrums relating to inductive cruciate ligament (ACL) injury in sport: recent evidence and a personal reflection. Br J Sports Med 2013;47:367-72. [Crossref] [PubMed]
- Granan LP, Forssblad Grand, Lind M, et al. The Scandinavian ACL registries 2004-2007: baseline epidemiology. Acta Orthop 2009;80:563-vii. [Crossref] [PubMed]
- Granan LP, Bahr R, Lie SA, et al. Timing of anterior cruciate ligament reconstructive surgery and hazard of cartilage lesions and meniscal tears: a accomplice report based on the Norwegian National Knee Ligament Registry. Am J Sports Med 2009;37:955-61. [Crossref] [PubMed]
- Lee K, Siegel MJ, Lau DM, et al. Inductive cruciate ligament tears: MR imaging-based diagnosis in a pediatric population. Radiology 1999;213:697-704. [Crossref] [PubMed]
- Trivedi Five, Mishra K, Verma D. Pediatric ACL Injuries: A Review of Electric current Concepts. Open Orthop J 2017;11:378-88. [Crossref] [PubMed]
- Kocher MS, DiCanzio J, Zurakowski D, et al. Diagnostic operation of clinical examination and selective magnetic resonance imaging in the evaluation of intraarticular knee joint disorders in children and adolescents. Am J Sports Med 2001;29:292-6. [Crossref] [PubMed]
- Grindem H, Eitzen I, Engebretsen L, et al. Nonsurgical or Surgical Treatment of ACL Injuries: Knee joint Function, Sports Participation, and Knee joint Reinjury: The Delaware-Oslo ACL Cohort Study. J Bone Joint Surg Am 2014;96:1233-41. [Crossref] [PubMed]
- Dejour H, Bonnin G. Tibial translation after anterior cruciate ligament rupture. Ii radiological tests compared. J Bone Joint Surg Br 1994;76:745-9. [Crossref] [PubMed]
- Ardern CL, Ekås GR, Grindem H, et al. Prevention, diagnosis and management of paediatric ACL injuries. Br J Sports Med 2018;52:1297-8. [Crossref] [PubMed]
- Canavese F, Charles YP, Dimeglio A, et al. A comparison of the simplified olecranon and digital methods of assessment of skeletal maturity during the pubertal growth spurt. Bone Articulation J 2014;96-B:1556-60. [Crossref] [PubMed]
- Canavese F, Charles YP, Dimeglio A. Skeletal historic period assessment from elbow radiographs. Review of the literature. Chir Organi Mov 2008;92:one-6. [Crossref] [PubMed]
- Dvorak J, George J, Junge A, et al. Age determination by magnetic resonance imaging of the wrist in boyish male football players. Br J Sports Med 2007;41:45-52. [Crossref] [PubMed]
- Wybier M, Bossard P. Musculoskeletal imaging in progress: the EOS imaging organization. Articulation Bone Spine 2013;lxxx:238-43. [Crossref] [PubMed]
- Gicquel P, Giacomelli 1000, Karger C, et al. Développement embryonnaire et croissance normale du genou. Rev Chir Orthopédique 2007;(93):3S100-102.
- Baxter MP. Cess of normal pediatric articulatio genus ligament laxity using the genucom. J Pediatr Orthop 1988;viii:546-50. [Crossref] [PubMed]
- McCarthy MM, Tucker South, Nguyen JT, et al. Contact stress and kinematic analysis of all-epiphyseal and over-the-top pediatric reconstruction techniques for the anterior cruciate ligament. Am J Sports Med 2013;41:1330-9. [Crossref] [PubMed]
- Seil R, Weitz FK, Pape D. Surgical-experimental principles of anterior cruciate ligament (ACL) reconstruction with open growth plates. J Exp Orthop 2015;two:xi. [Crossref] [PubMed]
- Moksnes H, Engebretsen L. The ESSKA paediatric anterior cruciate ligament monitoring initiative. Human knee Surg Sports Traumatol Arthrosc 2016;24:680-seven. [Crossref] [PubMed]
- Pennock AT, Ho B, Parvanta K, et al. Does Allograft Augmentation of Small-Bore Hamstring Autograft ACL Grafts Reduce the Incidence of Graft Retear? Am J Sports Med 2017;45:334-8. [Crossref] [PubMed]
- Momaya AM, Beicker C, Siffri P, et al. Preoperative Ultrasonography Is Unreliable in Predicting Hamstring Tendon Graft Diameter for ACL Reconstruction. Orthop J Sports Med 2018;6:2325967117746146 [Crossref] [PubMed]
- Micheli LJ, Rask B, Gerberg 50. Anterior cruciate ligament reconstruction in patients who are prepubescent. Clin Orthop 1999;40-vii. [Crossref] [PubMed]
- Goddard Grand, Bowman N, Salmon LJ, et al. Endoscopic Anterior Cruciate Ligament Reconstruction in Children Using Living Donor Hamstring Tendon Allografts. Am J Sports Med 2013;41:567-74. [Crossref] [PubMed]
- Heath EL, Salmon LJ, Cooper R, et al. 5-Year Survival of Pediatric Anterior Cruciate Ligament Reconstruction With Living Donor Hamstring Tendon Grafts. Am J Sports Med 2019;47:41-51. [Crossref] [PubMed]
- Engebretsen L, Svenningsen S, Benum P. Poor results of inductive cruciate ligament repair in adolescence. Acta Orthop Scand 1988;59:684-6. [Crossref] [PubMed]
- Mohtadi N, Grant J. Managing anterior cruciate ligament deficiency in the skeletally young individual: a systematic review of the literature. Clin J Sport Med 2006;xvi:457-64. [Crossref] [PubMed]
- Yoo WJ, Kocher MS, Micheli LJ. Growth plate disturbance after transphyseal reconstruction of the anterior cruciate ligament in skeletally immature adolescent patients: an MR imaging study. J Pediatr Orthop 2011;31:691-vi. [Crossref] [PubMed]
- Chotel F, Seil R. Growth disturbances after transphyseal ACL reconstruction in skeletally immature patients: who is more at run a risk? Young child or adolescent? J Pediatr Orthop 2013;33:585-6. [Crossref] [PubMed]
- Frosch KH, Stengel D, Brodhun T, et al. Outcomes and risks of operative treatment of rupture of the anterior cruciate ligament in children and adolescents. Arthroscopy 2010;26:1539-50. [Crossref] [PubMed]
- Wilmes P, Lorbach O, Chotel F, et al. Ersatzplastik des vorderen Kreuzbandes bei offenen Wachstumsfugen. Arthroskopie 2009;22:35-44. [Crossref]
- Shea KG, Appel P, Pfeiffer R. ACL injuries in paediatric and adolescent patients. Sports Med 2003;33:455-71. [Crossref] [PubMed]
- Robert H, Bonnard C. The possibilities of using the patellar tendon in the treatment of anterior cruciate ligament tears in children. Arthroscopy 1999;fifteen:73-6. [Crossref] [PubMed]
- Claes S, Vereecke E, et al. Anatomy of the anterolateral ligament of the human knee. J Anat 2013;223:321-8. [Crossref] [PubMed]
- Sonnery-Cottet B, Vieira TD, Ouanezar H. Anterolateral Ligament of the Genu: Diagnosis, Indications, Technique, Outcomes. Arthroscopy 2019;35:302-three. [Crossref] [PubMed]
- Chotel F, Henry J, Seil R, et al. Growth disturbances without growth arrest after ACL reconstruction in children. Knee Surg Sports Traumatol Arthrosc 2010;18:1496-500. [Crossref] [PubMed]
- McIntosh AL, Dahm DL, Stuart MJ. Anterior cruciate ligament reconstruction in the skeletally immature patient. Arthroscopy 2006;22:1325-30. [Crossref] [PubMed]
- Nwachukwu BU, McFeely ED, Nasreddine A, et al. Arthrofibrosis after anterior cruciate ligament reconstruction in children and adolescents. J Pediatr Orthop 2011;31:811-vii. [Crossref] [PubMed]
- Pauvert A, Robert H, Gicquel P, et al. MRI study of the ligamentization of ACL grafts in children with open growth plates. Orthop Traumatol Surg Res 2018;104:S161-7. [Crossref] [PubMed]
- Geffroy L, Lefevre N, Thevenin-Lemoine C, et al. Return to sport and re-tears later on anterior cruciate ligament reconstruction in children and adolescents. Orthop Traumatol Surg Res 2018;104:S183-8. [Crossref] [PubMed]
- Coleman BD, Khan KM, Maffulli N, et al. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Written report Group. Scand J Med Sci Sports 2000;ten:2-11. [Crossref] [PubMed]
- Pediatric ACL: Understanding Treatment Options (PLUTO) NCT02772770. Available online: https://clinicaltrials.gov/ct2/show/report/NCT02772770
doi: x.21037/aoj.2019.06.02
Cite this article as: Seil R, Cucchi D, Ninulescu C, Dor J, Mouton C. Anatomic inductive cruciate ligament reconstruction for adolescent patients with open physis. Ann Joint 2019;iv:31.
Source: https://aoj.amegroups.com/article/view/5243/html
0 Response to "Anatomic Posterior Cruciate Ligament Reconstruction State of the Art"
Post a Comment